Health is another factor that connects education and poverty. Low-income students’ poorer health relative to their better-off peers –physically , mentally and emotionally – and their lack of consistent access to preventive and remedial care combine to make them much more likely to miss school and to be less attentive while in class, which work to widen existing achievement gaps.
Required Reading
- Janet Currie “Healthy, Wealthy, and Wise? Socioeconomic Status, Poor Health in Childhood, and Human Capital Development,” Journal of Economic Literature, 47 #1, March 2009, 87-122. Currie links together various data on family consumption of goods, leisure, income, and others to illustrate how socioeconomic status affects child health, and then relates health to educational and labor outcomes. Evidence suggests that fetal health is one of the most important drivers of child health, leading her to highlight the need for better pre-natal care and to assert that such investments would lead to better education and labor outcomes.
- Neeta Thakur, Sam S. Oh, Elizabeth A. Nguyen, et al (2013). Socioeconomic Status and Childhood Asthma in Urban Minority Youths. American Journal of Respiratory and Critical Care Medicine 188(10): 1202-1209. Rates of asthma are particularly high among Latino and African-American children. Moreover, as the authors of this study document, children with asthma tend to have lower annual household incomes and lower socioeconomic status compared to children without asthma, due in part to those children’s their heightened exposure and their lack of access to medical care, which make it more likely for asthma to be undiagnosed. Low-SES children and families also tend to struggle more with stress, another driver of asthma, which is covered in Mirra and Rogers’ The Negative Impact of Community Stressors on Learning Time: Examining Inequalities between California High Schools.
- Students in need of vision, hearing, and speech/language support, and poverty related barriers to accessing these services (2016). BCTF Research/Committee for Action on Social Justice. This survey was designed to help researchers understand the challenges teachers face when students in their classroom suffer from vision and hearing problems. When asked how many of their students are in need of vision care, teachers report gaps between low income and high income students of 33% with respect to vision and 27.3% for hearing. The survey also found that teachers felt their effectiveness was impeded by “long wait-lists for diagnostic and treatment services” when teaching low-income students, and by a lack of resources to help families address these problems. According to Jaggernath, Overland, Ramson, Kovai, Chan, and Naidoo in a separate report, Poverty and Eye Health, those with poor eye health are more likely to have lower literacy levels, to be unemployed and have lower annual incomes, so it is important for teachers and schools to be equipped with proper resources to address eye health.
- Immunizations: Early Childhood (2014). U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. Child Health USA 2014. Substantial increases in the percentage of children who are immunized represent important progress in public health since the early 1900s, yet there is a racial gap existing today in those who are vaccinated. Black children are less likely than their white counterparts to receive the full set of recommended vaccinations. Still, children of families living below the poverty level and Hispanic and black children have lower rates of vaccination than white children. This report by the US Department of Health and Human Services suggests that reducing the costs to families of vaccinations and linking immunization to Women, Infants and Children services and to home visiting programs will increase rates of vaccinations among these populations.
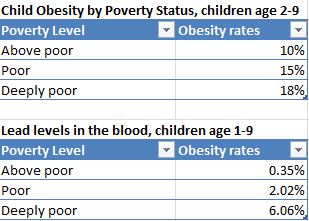
- Anna Aizer, Janet Currie, Peter Simon, Patrick Vivier (2015). Lead Exposure and Racial Disparities in Test Scores. Unpublished/Work in Progress. This study explores another possible cause for low test scores among low-income and minority students – lead exposure. After analyzing the test scores of roughly 57,000 students in Rhode Island, the authors found that the highest lead levels were present in students on the lower tail of the distribution. The study also reveals that lead exposure was disproportionately common in black neighborhoods and among children of less educated mothers. Even though lead levels overall have fallen in recent decades, children growing up in poverty, and especially racial and ethnic minorities, continue to suffer from lead exposure. Given that lead can substantially impede a child’s education, with lead exposure in preschool having a negative effect on future academics; it is a concern that must be addressed by targeted environmental regulations.
Optional Reading
- Ana B. Ibarra (2016). California’s Glaring Shortage of School Nurses. Kaiser Health News. A new recommendation by California pediatricians has raised public awareness regarding the need for more school nurses. School nurses can help manage chronic diseases, assist in obesity prevention, participate in emergency preparedness, and prevent chronic absenteeism. And as per Rodriguez, Rivera, et al, “School Nurses’ Role in Asthma Management, School Absenteeism, and Cost Savings: A Demonstration Project,” student attendance improved and family visits to the emergency room declined with the employment of school nurses. The American Academy of Pediatrics recommends that each school has at least one school nurse on campus, but the shortage of nurses in California makes it hard to meet these standards.
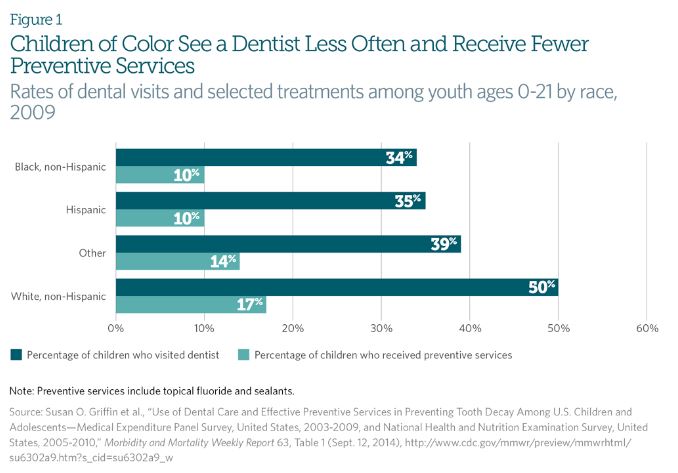
- Stephanie L. Jackson, William F. Vann Jr., Jonathan B. Kotch, Bhavna T. Pahel, Jessica Y. Lee (2011). Impact of Poor Oral Health on Children’s School Attendance and Performance. American Journal of Public Health 101(10), 1900-1906. Children with dental pain – which is an indication of an untreated oral health problem, such as a cavity or abscess — are more likely to be absent from school, which is linked to poor school performance. This study suggests that increasing students’ access to dental care would help improve academic achievement among children experiencing dental pain.
- Dana Charles McCoy, C. Cybele Raver, Patrick Sharkey (2015) Children’s Cognitive Performance and Selective Attention Following Recent Community Violence. Journal of Health and Social Behavior, 1-18. This study finds a link between children’s exposure to community violence and their ability to make good decisions. The authors discover that witnessing community violence can cause students to be more impulsive, which results in negative school performance. The impacts of community violence are influenced by the physical distance the student is to the crime; the closer the student is to the crime physically, the more likely he or she will perform negatively on assessments. McCoy and her peers thus point to community violent crime as one driver of income- and race-based disparities in school achievement.
- Nicole Mirra and John Rogers (2015). The Negative Impact of Community Stressors on Learning Time: Examining Inequalities between California High Schools. Annenberg Institute for School Reform: Voices in Urban Education (40). Community stressors in low-income schools can reduce instructional time by up to two weeks of the academic year. These stressors can include students’ need to care for family members, economic hardship, lack of medical care, hunger, immigration issues, community violence, and others. Students who experience these stressors are more likely than their less-stressed peers to lose focus or cause disruption during instruction. Time lost due to these factors contributes to gaps in educational opportunity.
Graphics/Data
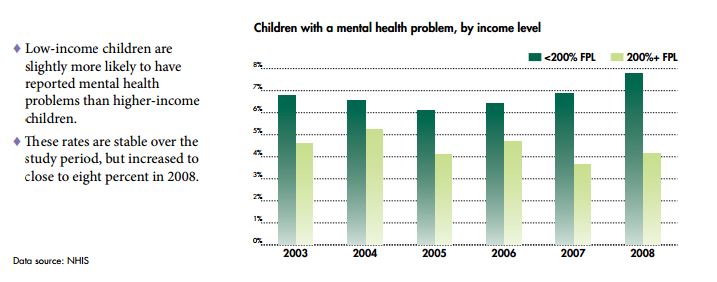
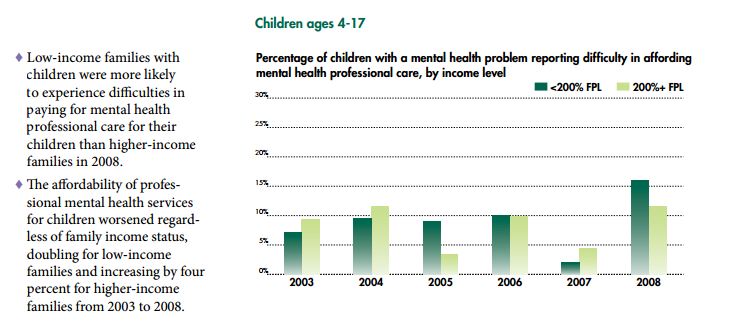
- Mental Health Chart book: Tracking the Well-being of People with Mental Health Challenges (2012). National Center for Children in Poverty. This publication outlines the state of mental health in the United States among both children and adults, including the prevalence of mental health problems, prescriptions to treat them, emergency room visits, hospitalizations, health insurance coverage, and more. Data show income-based gaps with respect to mental health problems and access to care/treatment that grew between 2003 and 2008.
- Young Children in Deep Poverty Fact Sheet (2016). National Center for Children in Poverty. These data, which compare basic health status among children living in deep poverty (defined as half the Federal Poverty Level or below), poverty (100% of the FPL) and above-poverty households, show that children classified as deeply poor are nearly twice as likely to be obese as are children who are classified as above poor. Other statistics show race- and poverty-based disparities in lead levels, stress, developmental delays, and other important indicators of health and well-being.
- Jane Koppelman and Rebecca Singer Cohen (2016). Dental Health is Worse in Communities of Color. The Pew Charitable Trusts: Dental Campaign. These statistics illuminate the racial gaps that exist in dental treatment in the United States. Specifically, children of color are more likely to suffer from tooth decay but less likely to visit a dentist and receive preventive dental service and sealants.
Movie
- Rich Hill. This Sundance award-winning documentary, which tracks a year in the lives of three high school boys in the town of Rich Hill in the Missouri Ozarks, shines a harsh spotlight on the connections between their families’ and community’s poverty and resulting health problems. Among health-related challenges that can impede academic achievement are the dearth of available nutritious options, the prevalence of smoking even among young teens and, in perhaps most visible, triggers of mental health problems combined with few supports to address them, which is exacerbated by the kids’ and town’s isolation. Several scenes depict these problems playing out in the school and the teachers’ and principal’s lack of resources to address them.
Book club
- Social Injustice and Public Health (2013). Barry S. Levy and Victor W. Sidel (editors). Oxford University Press. As the authors of this scholarly compendium on the many connections between poverty and health note, we live in the richest nation on earth, yet 15% of the US population live below the poverty line, and nearly one in four children is growing up in poverty. These children and their families have less access to medical care and are less informed about health threats and how to counter them or to navigate our increasingly complex health care system to get the services they need. For these and many other reasons, poor children growing up in the US – more so than in other Western countries — are much more likely than their non-poor counterparts to be injured, to develop illnesses, to become disabled, and even to die early. Poverty is driving a public health crisis in America that urgently demands policy action.
Discussion Questions
- Poverty has clear influences on health-related factors from children’s earliest years, even before birth. What are key strategies the US could adopt, including legislation we could enact, that would help reduce these impacts? Which would you prioritize?
- The BCTF Research study on teachers’ perspectives on their students’ health issues documented the challenges they face when working with low income students who have vision and hearing problems. Numerous other studies have shown that these problems affect student performance in school. Should teachers and schools be responsible for addressing student’s health needs? If so, how to balance that with parents’ responsibilities? How can schools better support families facing health issues?
- Many of these studies point to health factors directly or indirectly affecting test scores and educational outcomes. How do these factors legitimize (or fail to legitimize), the push for standardized testing and accountability in education?